
Case Study
Possible Link Between COVID-19 Vaccination and Autoimmune Disorders
Do SARS-CoV-2 mRNA vaccines make you more susceptible to autoimmune disorders like acquired hemophilia? Researchers in Taiwan explore cases for insights
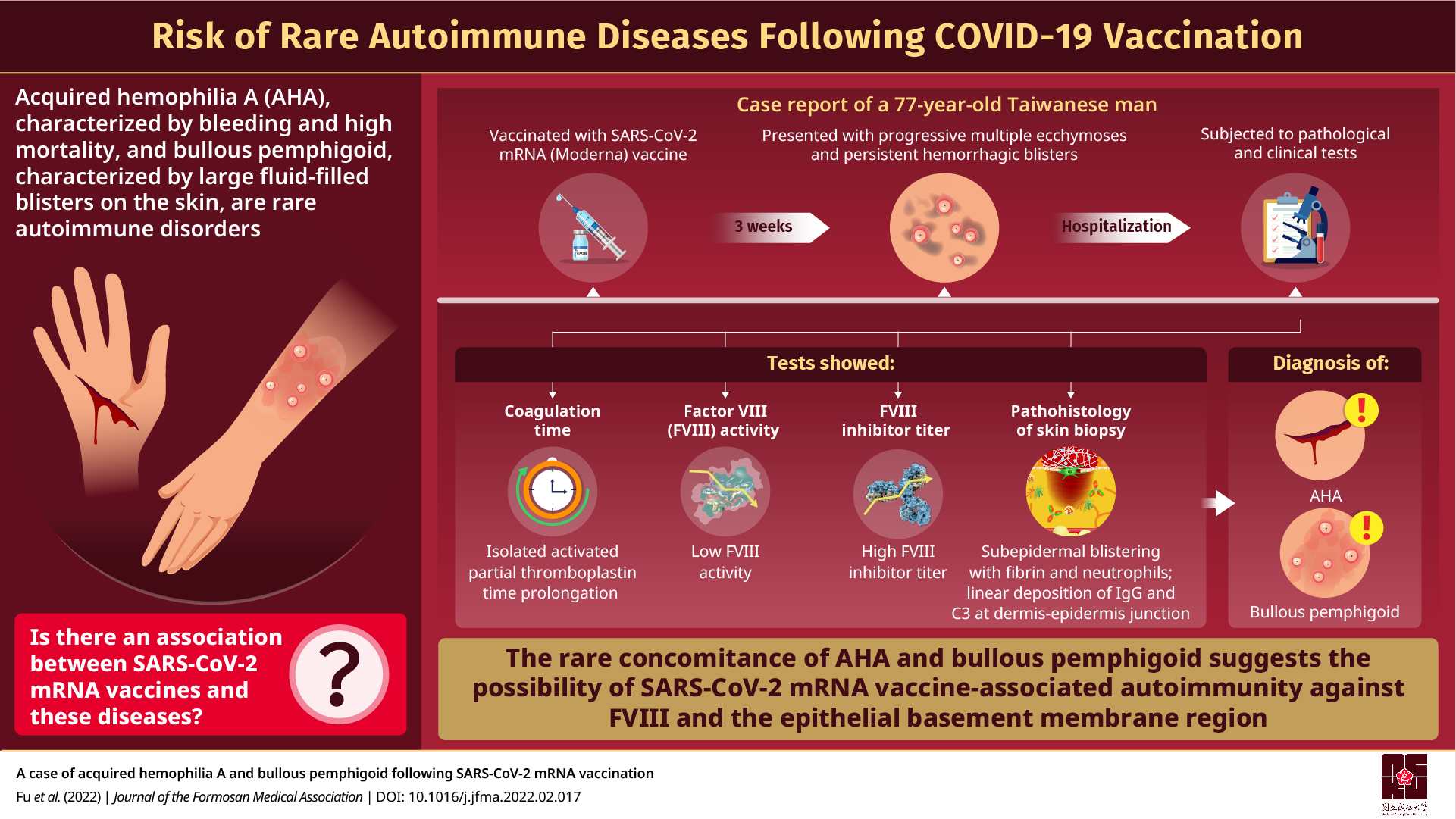
Considered a rare autoimmune disease, acquired hemophilia A (AHA) has been associated with bleeding and high death rates. In AHA, there is a breakdown of the immune system due to genetic and environmental factors. Do infectious diseases like COVID-19 increase the risk of AHA? Researchers from Taiwan report a rare case of concomitant occurrence of AHA and an autoimmune skin blistering disorder following COVID-19 vaccination raising concerns about a possible connection.
When the body’s immune system turns on itself and attacks the body’s healthy cells and organs, we have a problem—autoimmune disorders. A rare entrant in the list of autoimmune disorders is acquired hemophilia A (AHA) in which spontaneous bleeding occurs in patients with no previous history of the condition. Although AHA is often associated with significant mortality, owing to its rarity, there is very little data on the physiological processes associated with it.
Do other diseases that involve considerable immune suppression, for instance viral infections, have an association with AHA? A group of researchers led by Dr. Ya Ting Hsu and Dr. Peng Chan Lin of the NCKU Hospital, Taiwan, have recently reported a case that suggests there could be such a possibility.
In their case report made available online on March 14, 2022 in the Journal of the Formosan Medical Association, the researchers detail the symptoms, diagnosis, and treatment of a 77-year-old Taiwanese man who presented with bruised-looking skin on his forearms and legs along with bleeding blisters on his hands and trunks three weeks after receiving the second dose of the mRNA Moderna vaccine against the viral infection, COVID-19. Pathological and clinical tests, including blood coagulation factor VIII (FVIII) titer and FVIII inhibitor level estimation, and a skin biopsy confirmed AHA concomitantly occurring with bullous pemphigoid, a rare autoimmune skin disease. “Our patient was simultaneously diagnosed with AHA and bullous pemphigoid, which is very rare. Multiple studies have indicated that medications or vaccines play a role in inducing bullous pemphigoid, but the progression to this condition is still unclear. Although the causality and pathogenesis of the autoimmune conditions in our case have not been fully confirmed yet, we reported this case to raise awareness of this rare phenomenon following SARS-CoV-2 mRNA vaccine administration,” explains Dr. Hsu.
mRNA vaccines have been the first line of defense against SARS-CoV-2-induced COVID-19 across the world in recent times. Awareness of autoimmune diseases associated with these vaccines can help physicians provide timely treatment and prevent significant morbidity and mortality in patients. “There are several questions that need to be asked if we are to understand vaccine-related autoimmune diseases. For example, do patients with known autoimmune diseases have a higher risk of developing vaccine-related autoimmune disease? Can they receive a SARS-CoV-2 mRNA vaccine safely? Will the vaccine trigger flare up of an existing autoimmune disease? Will these patients be treated differently?” observes Dr. Lin, while explaining the need for extensive, timely, and honest reporting of relevant incidents.
If more autoimmune diseases following SARS-CoV-2 mRNA vaccine administration are reported, further investigation into their pathogenesis can be made. This can then help identify the potential groups at the risk of developing autoimmune diseases following vaccination.
So, are there any more cases reported till date? Although this was the only case reported for concomitant occurrence of AHA and bullous pemphigoid, the researchers cite six other vaccine-related cases of AHA reported since 2021. The six cases shared characteristics. Firstly, the SARS-CoV-2 mRNA vaccine administered to these six patients was either Moderna or Pfizer-BioNTech. Secondly, a faster response to treatment along with shorter remission time when compared with non-vaccine associated AHA was noted in all six cases. The symptoms of all except one patient were cured within a span of four weeks upon administering immunosuppression treatment. Thirdly, all the cases reported were of AHA and no cases of acquired hemophilia B was detected. “However, some differences were also noticed in the six cases,” Dr Hsu added. “The tendency of bleeding varied from four days to three weeks after vaccination.”
The researchers further note that apart from the six COVID-19 vaccination-related cases, two more AHA cases following influenza vaccination have been reported, even though the antigens used in the two vaccines are very different.
Although these findings point to a possible association between SARS-CoV-2 mRNA vaccines and autoimmune diseases like AHA, the researchers emphasize the necessity of further studies to conclusively prove a causal link between the two. For now, however, they strongly recommend the timely reporting of such cases so that the short-term and long-term side effects of our best defense against COVID-19, i.e., mRNA vaccines, is better understood and patient management improved for better outcomes.
Reference
AuthorsPei-An Fua, Chien-Wei Chenb, Ya-Ting Hsuc, Kai-Che Weid, Peng-Chan Line, Tsai-Yun Chenc
Affiliations
a Department of Internal Medicine, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, Taiwan
b Education Center, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
c Division of Hematology, Department of Internal Medicine, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, Taiwan
d Department of Dermatology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
e Department of Oncology, National Cheng Kung University Hospital, College of Medicine, National Cheng Kung University, Tainan, Taiwan
Key Academics
About Dr. Ya-Ting HsuDr. Ya-Ting Hsu is a medical doctor associated with the Department of Internal Medicine at NCKU Hospital, Taiwan. Dr. Hsu has published 18 scientific manuscripts and been cited over 27 times.
Dr. Peng-Chan Lin is an Associate Professor in the Department of Oncology at NCKU Hospital, Taiwan. He has published over 69 documents and been cited over 677 times.